SHARE THIS ARTICLE:
PA – House Majority Policy Comm. Hearing
Testimony/Recommendations to: The House Majority Policy Committee Hearing on Combating Lyme Disease Dec. 2, 2009 Worcester PA
Representative Mike Sturla, Chairman; Representative Matthew Bradford, Host
Thank you all for the opportunity to testify on this very important issue, Lyme disease.
As background: The Lyme Disease Association (LDA) is all-volunteer national non profit devoted to education, research funding, prevention & patient support. It has 34 allied organizations nationwide, including a PA affiliate, LDASEPA, and a PA Chapter, which primarily focuses on education. LDA is part of the 2009 Combined Federal Campaign (CFC) as a national charity. We have presented 10 fully CME accredited scientific conferences, 8 jointly sponsored by Columbia University, 3 held in Philadelphia, which is also being considered as our 2010 conference venue.
LDA’s LymeAid 4 Kids fund, developed with author Amy Tan, dispenses money for children without insurance − 19 Pennsylvania children have benefited to date from this fund. LDA provides research grants coast-to-coast and has funded several projects in Pennsylvania connected to researchers at Fox Chase Cancer Center, University of Pennsylvania, Edinboro University of Pennsylvania, and University of Pittsburg School of Nursing and has partnered with its CT affiliate, TFL, to endow the first center in the world at Columbia to study chronic Lyme in 2007. That same year, I was invited to speak at Ft. Collins, Colorado, to the Centers for Disease Control & Prevention’s (CDC) Vector-Borne Diseases Division where Lyme is studied.
LDA is an Environmental Protection Agency (EPA) PESP partner and sits on a working group with EPA and with CDC. We are currently developing measures to help reduce children’s exposure to Lyme disease. We hope to use existing tools such as the LDA website which is also linked with EPA’s site, to provide parents with educational materials to complement an EPA-funded prevention video and an interactive video game for kids being developed by NJ Medical School in collaboration with LDA. The parent materials may contain links to composition/effectivity of pesticides and property management techniques for schools. We are also seeking to publish with the National Association of School Nurses, possibly using existing publications to publish the prevention message to schools.
A CDC study of New Jersey children K-12 with Lyme showed the median number of missed school days was 140; median duration of home instruction, 153 days; 78% of parents said their children experienced a fall in grade point average during illness; 79% experienced a decrease in friends; “…isolated from social groups and missing out on cultural, sports and social activities….School performance of nearly all patients fell sometimes drastically, and in several instances, was said to interfere with selection by colleges and universities.”i A study at Columbia demonstrated a drop of 22 IQ points in a student with Lyme disease, later reversed with treatment.ii
According to CDC, boys & girls ages 5-9 are at the greatest risk of acquiring Lyme,iii the most prevalent vector-borne disease in the US today, reported in all 50 states. From 1990 through 2008, PA ranked #2 nationwide with 51,266 reported Lyme cases. CDC states only 10% of cases that meet CDC surveillance criteria are reported,iv meaning over 1⁄2 million (512,660) PA residents developed Lyme that met the surveillance criteria over that time, a number that includes my now late parents.
That number is only a fraction of cases that probably occurred, since CDC’s surveillance criteria are meant for comparing cases of Lyme in one state to another and don’t include cases clinically diagnosed by physicians − meaning cases without an EM rash or without a positive test. Numbers in PA are sharply rising, with 2009 numbers already more than double 2008 total numbers (7,540/3602).

The situation isn’t likely to improve soon. Deforestation, increase in deer herds and climate changes are said to be contributing to increased tick populations and expanded tick ranges, increasing disease burden. According to Penn State College of Agricultural Sciences, a 1960’s survey in PA identified 20 tick species in-state, with deer ticks found only in Philadelphia County. Furthermore, in the late 80s, deer ticks were mostly limited to the southeast corner, the north central region around Elk State Forest and the Presque Isle peninsula in Erie but now they are established in more areas around the state and 25 species have been identified.
Ninety percent of tick identification submissions to Penn State consist of 4 ticks, 3 of which transmit many tick-borne diseases to humans:
1) American dog tick (RMSF, tularemia, ehrlichiosis, tick paralysis);
2) blacklegged tick [deer tick] (Lyme, babesiosis, anaplasmosis, Powassan encephalitis, tick paralysis, tularemia, bartonellosis); and
3) lone star tick (ehrlichiosis, tularemia, RMSF, tick paralysis, Q fever, and STARI). Southern Tick- Associated rash illness (STARI), looks and acts like Lyme, sometimes has the same bull’s eye rash, is treated the same way, but there is no test for it. The lone star tick is much more aggressive than a deer tick and will stalk you from 50 feet away. Tick-borne diseases are increasing in general, but Lyme itself increased 250% nationwide from 1993 through 2008.
Lyme is now found in 65 countries worldwide. A UN commissioned study indicates ticks in Sweden have moved almost as far north as the Arctic Circle and are being found in January. Reports from researchers and patients seem to confirm that latter finding in the Northeast. In January 2005, my daughter pulled a fully engorged deer tick off my then 5-year old granddaughter’s ear. It was 25°.
Two items greatly influence the ability and willingness of doctors to diagnosis and treat Lyme patients, including children − the first is the CDC surveillance criteria. Despite CDC’s warning that the surveillance criteria are NOT intended for diagnosis, treatment, or insurance reimbursement, but are only intended for disease surveillance reporting, most doctors are inappropriately using them to diagnose and treat and insurance companies are using them to deny treatment reimbursement. The CDC criteria for an endemic region are: an EM rash (plus a required test in a non-endemic region), OR major system involvement plus positive blood work.
Although CDC criteria are for surveillance purposes only, patients who do not meet that criteria must scramble to find physicians willing to risk making a clinical diagnosis for Lyme disease, one based on symptoms, history, ruling out other diseases, one which does not require a positive test for diagnosis. Problems about diagnosis are fueled by unreliable Lyme testing that is 40-60% accurate, v and by the fact that less than 50% of people develop the classic bull’s eye rash. vi
The second item influencing doctors’ ability and willingness to treat is the Infectious Diseases Society of America (IDSA) Lyme treatment guidelines (“Guidelines”). They recommend against any long-term treatment for chronic Lyme; against entire classes of antibiotics; against alternative treatments; against some supplements; and against individual physician discretion in diagnosis and treatment. IDSA says there is NO chronic Lyme disease.
Despite a disclaimer that says they are NOT mandatory, actual experiences demonstrate the Guidelines have become de facto law. Medical boards, health departments, hospitals, insurers, schools, pharmacists, and IDSA doctors themselves often hold that position, leading to doctor prosecution and inability of patients to get medical care for Lyme disease. The abuse has been so blatant that Connecticut State Attorney General Richard Blumenthal initiated an investigation of the IDSA Guidelines’ development process.
In a 2008 settlement Agreement with IDSA, Mr. Blumenthal stated: “This agreement vindicates my investigation−finding undisclosed financial interests…held by several of the most powerful IDSA panelists. The…panel improperly ignored or minimized consideration of alternative medical opinion and evidence regarding chronic Lyme disease, potentially raising serious questions about whether the recommendations reflected all relevant science…The IDSA’s Lyme guideline process lacked important procedural safeguards….”vii IDSA had to form a new panel, which heard testimony in July 2009, re-looking at the guidelines, but it again excluded chronic Lyme treating doctors as panel members.
There are other Lyme treatment guidelines which differ from IDSA’s, which do allow doctor discretion in diagnosis and treatment, and do recognize that Lyme sometimes requires more than a short course to make people better. They provide the basis for a second standard of care for Lyme disease. Published by the International Lyme & Associated Diseases Society (ILADS), a professional medical and research organization,viii they’re ignored by IDSA and often not disclosed as an option by doctors to patients. They are published on the Department of Health and Human Services National Guidelines Clearing House website, recognizing them as being evidenced-based.ix
ILADS’ approach recognizes that patients who are not diagnosed quickly or not treated appropriately can become chronically ill− one study shows that Lyme patients suffer a degree of disability equal to that of patients with congestive heart failure.x Yet many of these patients, often multi-members of one family,xi now have to travel many hours outside Pennsylvania to find care for their Lyme. They don’t have the resources nor the health to fight the vested interests stacked against them, which is why legislation is often necessary to protect doctors who treat, ensuring that in-state treating doctors cannot be prosecuted for unprofessional conduct solely for providing long-term treatment based on clinical judgment. Rhode Island, Connecticut and California have passed protective legislation. Massachusetts, Minnesota, and Pennsylvania have introduced it, with another state about to do so.
Despite two standards of care for Lyme, physicians continue to be monitored by insurance companies who say stop prescribing antibiotics for Lyme disease or leave the insurance plan. Some doctors then leave the plan voluntarily, others are forced out. Some continue treating patients without accepting insurance. Other physicians fear scrutiny from the insurance companies and stop treating Lyme disease entirely, leading to a scarcity of physicians.
Patients lack of insurance coverage leads to limited courses of antibiotics, often not effective in eradicating the Lyme bacterium, which has the ability to hide inside cells, kill human lymphocytes and certain B cells and to change into other forms. Legislation requiring insurance companies to cover patients for Lyme treatment has been passed in Rhode Island and Connecticut and has been introduced in Pennsylvania. The legislature should pass Pennsylvania Lyme bills HB 894 & SB346 which provide for doctor protection, insurance coverage, and creation of a task force.
Most of the opposition to Lyme doctor protection legislation comes from the IDSA itself. You have heard how doctors who don’t follow IDSA Guidelines but use their own clinical skills to diagnose and treat face medical board discipline, hospital privilege/post revocation, and insurance plan exclusion if they do not march lockstep with IDSA, creating a “chilled” treatment climate.
IDSA sometimes cites development of antibiotic resistance for opposing legislation, despite resistance most often developing due to under usage rather than over usage of antibiotics. The Union of Concerned Scientists feels a significant cause of resistant bacteria may be an estimated 70% of antibiotics in the U.S. being fed to healthy pigs, cows, and chickens to promote growth and prevent disease.xii Antibiotic resistant strains often spread due to improper hygiene by medical personnel in hospitals. IDSA also ignores the fact that other diseases are allowed long-term treatment with antibiotics including tuberculosis, Q fever endocarditis, and even acne. Terribly sick Lyme patients are singled out to be left without treatment because of undocumented accusations of resistance due to treating sick people.
IDSA even opposes federal legislation (HR 1179 C. Smith [NJ] 86 co-sponsors, S 1352 C. Dodd [CT] 8 co-sponsors), Lyme & Tick-Borne diseases Prevention, Research and Education Act 2009, which provides much needed research funds − $100M over 5 years, particularly for an accurate test to help resolve many Lyme-related issues. IDSA indicates they do not like the constitution of a Lyme and tick- borne diseases federal advisory committee created by the bills because it contains patient and treating physician reps with different viewpoints, although many other diseases have that type of panel.
Following IDSA Guidelines can lead to delayed diagnosis and treatment. According to an actuarial study on Lyme costs, “37% of the financial costs of this disease is incurred before the correct diagnosis is made.” xiii A delay in diagnosis also leads to more chronic disease since the Lyme bacterium can get into the brain within 24 hours of a tick bite.xiv Chronic Lyme is more costly to patients physically, mentally, and financially. According to a 1998 CDC journal study, early Lyme costs* averaged $161 per patient and neurologic longstanding Lyme disease averaged $61,243.xv Chronic Lyme is also more costly to the state and federal government in terms of disability and education e.g., special services, home instruction, substitute teachers. xvi Allowing doctor discretion in diagnosing and treating can cut costs and most importantly, human suffering.
In 2009 LDA and its partner groups were successful in having language included in the US House Appropriations bill which passed the full House and includes the terms “chronic Lyme disease” and “persistence.” The language also passed the Senate Committee and is awaiting full Senate vote. Full passage will help Lyme patients receive the medical treatment they require.
Besides legislation, public and physician education is very important. LDA just received a copy of a letter from a western PA physician to his patient. The patient was bitten by something and had a possible bull’s eye rash. The doctor was unsure if Lyme was even in the county, checked with health department officials who said the reported cases there were not from within the county, although how that was determined is not stated. He thus determined Lyme was probably not endemic there. The doctor requested supporting info from the patient about Lyme in the area, although he did prescribe a minimal dose of medication. A quick check by me of the canine cases in that county reported by an IDEXX Veterinary Labs survey, an LDA corporate partner, shows 122 Lyme cases there in dogs, which are sentinels for the disease.
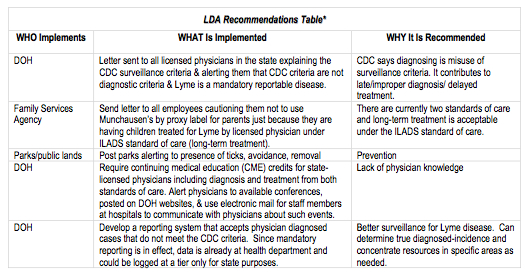
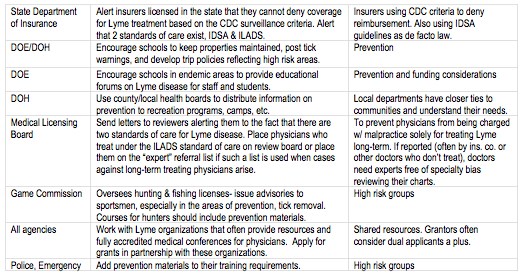
To help states educate and combat against tick-borne diseases, LDA has developed a table of general recommendations for states:
On Thanksgiving at my home last week, 4 of the 12 adults had been diagnosed with Lyme disease, 2 from NJ, 2 from PA. Another from PA will probably be diagnosed with Lyme and/or another tick-borne disease called anaplasmosis. All states need to take actions to prevent the further spread of Lyme and other tick- borne diseases which are devastating entire families and to help those already infected. No one is safe from these complicated infections.
Thank you.
i David Dennis, CDC, presented study in Wall Township, NJ, October 1992, Congressional meeting. Later pub. Lyme Times Children’s Educational Issue, ed. CALDA, Summer 2006.
ii Brian Fallon MD The Underdiagnosis of Neuropsychiatric Lyme Disease in Children & Adult, The psychiatric Clinics of North America, Vol.21, No.3, Sept.1998.
iii Centers for Disease Control & Prevention, Average Annual Incidence of Reported Cases of Lyme Disease by Age Group & Sex, https://www.cdc.gov/ncidod/dvbid/lyme/ld_MeanAnnualIncidence.htm.
iv Paul Meade, CDC, Herald News 5-4-04, Jessica Adler.
v P. Coulter et al, J. Clin Microbiol. 2005 Oct.; 43(10): 5080-4 Two Year Evaluation of Borrelia burgdorferi Culture and Supplemental Tests for Definitive Diagnosis of Lyme Disease. Lancet 1990, Journal of Clinical Investigation 1994 & S. Schutzer et al, JAMA Vol 282, No. 20 Borrelia Burgdorferi:Specific Immune Complexes in Acute Lyme Disease,Nov. 24,’99
vi R. Smith et al, Annals of Internal Medicine 2002;421:421-428, 477-479; A. Pachner, Reviews of Infectious Diseases-Vol. II, supplement 6 – September- October 1989 Neurologic Manifestations of Lyme Disease, the new “Great Imitator”; J.M. Johnson, Ph.D., Chief, Public Health, NPS Ticks and Disease. vii Office of the Connecticut Attorney General, press release, May 1, 2008.
viii Daniel Cameron, et al, Expert Review of Anti-infective therapy 2(1) Suppl. 2004
ix AHRQ, https://www.guideline.gov/.
x Connecticut Agricultural Experiment Station, “Summary of Tick Testing Results for 2003.” www.caes.state.ct.us.
xi CDC unpub. study data presented in Congressional forum, Wall NJ Oct 1992 (Later pub. in Lyme Times)
xii https://www.ucsusa.org/food_and_environment/antibiotics_and_food/myths-and-realities.
xiii Irwin Vanderhoof, Lyme Disease the Cost to Society, Contingencies January/Februray 1993.
xiv Steere, Allen, Mandel, Douglas, and Bennett’s Principals & Practices of Infectious Diseases, 4th ed. 1995. xiv Martin I. Meltzer The Cost Effectiveness of Vaccinating against Lyme Disease CDC Emerging Infectious Diseases; Vol.5, No.3; 1999 May-June;5(3)321-8. * This is in 1996 costs not adjusted. The following additional significant costs to society aren’t measured by this table: special education needs for children, disability, increased medical and insurance costs, and livestock losses, etc. Also, there are personal loses: friends, employment, self, esteem, domicile, and breakup of families.
xv Martin I. Meltzer The Cost Effectiveness of Vaccinating against Lyme Disease CDC Emerging Infectious Diseases; Vol.5, No.3; 1999 May- June;5(3)321-8. * This is 1996 costs not adjusted to 2007. The following additional costs to society aren’t measured by this table: special education needs for children, disability, increased medical and insurance costs, and livestock losses, etc. Also, there are personal loses: friends, employment, self, esteem, domicile, and breakup of families.
xvi Patricia Smith, Wall Township, NJ, Board of Education member NJ School District Study on Impact of Lyme Disease on School Districts presented in Washington DC Congressionally hosted meeting with CDC & NIH, March 12, 1992.
*LDA recommends that State agencies consult with patient groups within state and/or the national LDA to provide input into these areas since these groups can often provide a perspective the State does otherwise not have access to, and they can provide feedback from solutions other states may have attempted/implemented. ©Lyme Disease Association, Inc. 2005 www.LymeDiseaseAssociation.org PO Box 1438 Jackson, NJ 08527 888 366 6611